How can we help?
-

Request an Urgent Appointment
Click here if you have an Urgent medical Problem that cannot wait
-

Request a routine (Non- Urgent) Appointment
Please note this form is for pre-bookable routine appointments ONLY
-

Request a Nurse Appointment
Click here to submit a Nurse appointment request
-

I have an admin Request
Contact us about an administrative query and update your contact details
-

Promoting healthy behaviours
Understand the drivers of unhealthy behaviour and make healthy choices.
-

Order Repeat Medication
Use this link to order Repeat Medication. If you do not currently have an online account , you can register here
-
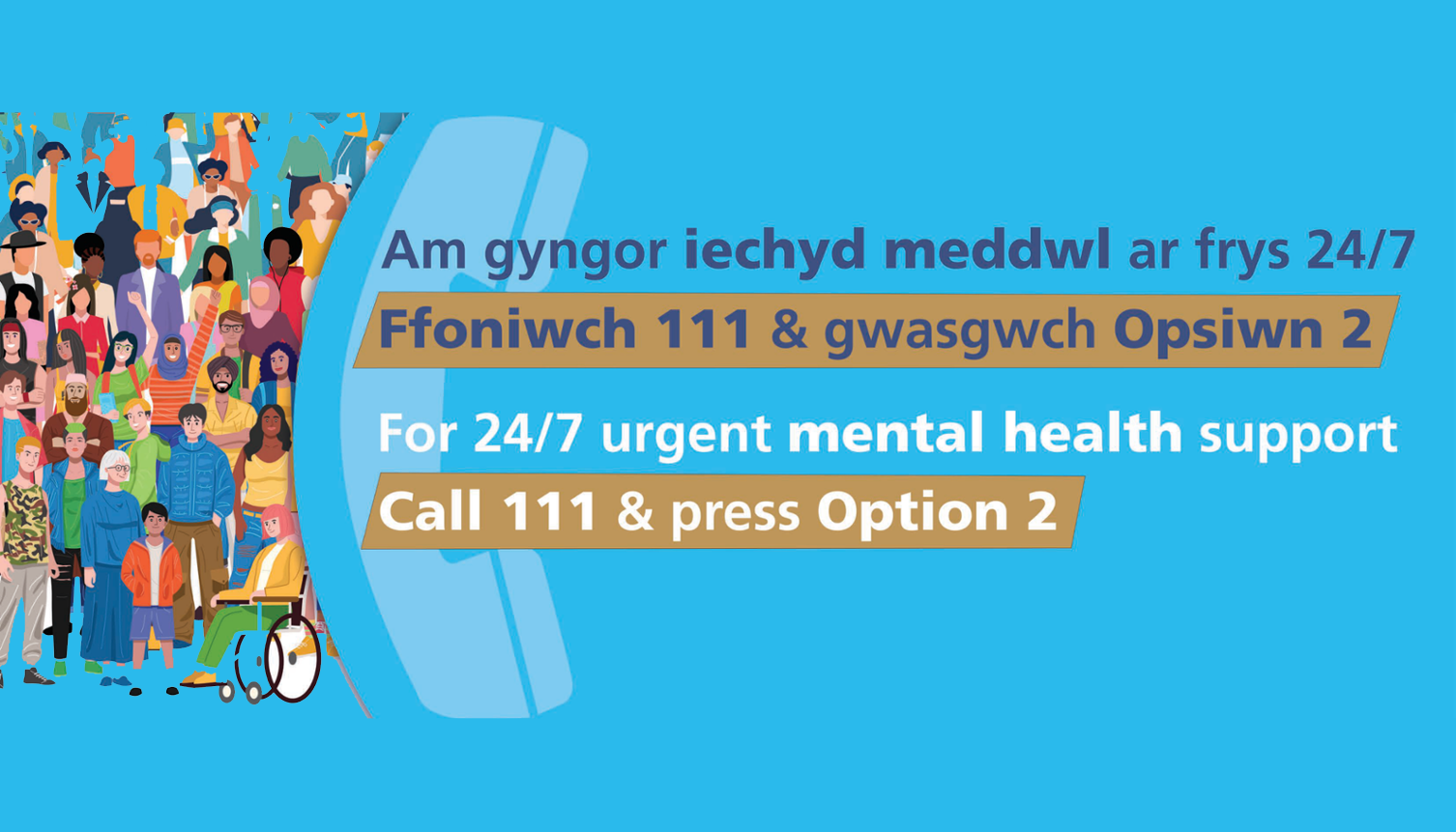
Urgent Mental Health Support - 24 hours a day, 7 days a week
We’re here 24 hours a day, seven days a week – offering urgent mental health support to people of all ages
-
Common Ailments Service
Get a consultation and free treatment for 27 common conditions at your local pharmacy
-

Help Us to Help You
From pharmacists to minor injury units and mental health helplines to online consultations, there are many ways to access the NHS in Wales. Find out more here
-

Health Resources
Find advice for conditions like back pain, coughs, headaches & more and access our video library.
Surgery Details
Church Surgery

Door Opening Times
| Monday | 08:00 - 18:00 | |
|---|---|---|
| Tuesday | 08:00 - 18:00 | |
| Wednesday | 08:00 - 18:00 | |
| Thursday | 08:00 - 18:00 | |
| Friday | 08:00 - 18:00 | |
| Weekend | Closed | |
Telephone Opening Times
| Monday | 08:00 - 18:30 | |
|---|---|---|
| Tuesday | 08:00 - 18:30 | |
| Wednesday | 08:00 - 18:30 | |
| Thursday | 08:00 - 18:30 | |
| Friday | 08:00 - 18:30 | |
| Weekend | Closed | |

